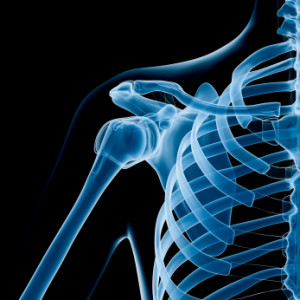
 What is the rotator cuff?
What is the rotator cuff?
The rotator cuff muscles consist of 4 small muscles that work together to keep the shoulder joint centred – supraspinatus (most commonly associated with a rotator cuff tear); infraspinatus and teres minor (the external rotators); and subscapularis (the internal rotator and least understood but arguably the most important).
Why is it important?
Imagine the shoulder joint as a golf ball sitting on a golf tee. It requires the small rotator cuff muscles closest to the joint to stabilise it so the larger muscles can move the arm efficiently.
What is shoulder impingement?
Impingement is the most common pathology seen in the shoulder, which involves the tendons and other soft tissues get squished under the acromion (a bony arch forming a roof above the shoulder joint).
How do we manage it?
The management largely depends on the cause. Often a muscle imbalance is created by repetitive use of the arm over shoulder height (throwers or swimming). The muscle imbalance can be associated with the scapula (resulting in scapula winging or lack of rotation control) which requires specific exercise to stabilise the shoulder blade region.
Additionally a muscle imbalance of the rotator cuff can be created by the pain associated with impingement symptoms. This can be identified via a physical assessment of active movement control versus passive range available and if clinically relevant to the symptoms will result in improvement within a 2 week period. Occasionally the acromion is shaped in a hook fashion which increases the chance of impingement and this can require surgery (acromioplasty) to shave away and make more space in the area.
The concept that muscle imbalance and fatigue can lead to shoulder impingement has been validated over the years, and supports the use of rotator cuff strengthening exercises as an effective treatment for shoulder impingement.