1. Rest completely
Tendon pain stems from the tendon not coping with a given load. Complete rest will only decrease the tendon’s capacity to tolerate load even further. Rather than completely resting, you should continue to place the tendon under a small amount of load that you know it will tolerate, and then slowly and progressively increase it over time.
2. Have ongoing passive treatments
Passive treatment such as massage, dry needling, ice, heat, TENS, ultrasound and interferential do not improve the tendon’s capacity to tolerate load, and therefore will usually not provide long lasting benefit. Some of these treatments can be helpful in the short term for pain relief if you aren’t coping, however it is understood that these treatments aren’t curative.


3. Have injection therapies
Injections directly into tendon tissues has not been shown to be effective in good clinical trials. In some cases, particular injections can actually have a detrimental effect to the tendon’s health long term. They should only be considered if the tendon has not responded to a well designed and implemented exercise-based program.
4. Ignore your pain
Once you have tendon pain, it is normal to expect some pain when you place load on the tendon. Just as you shouldn’t rest completely, you also shouldn’t push through large amounts of pain. A general guide is that pain more than 4/10 pain might indicate that the tendon isn’t coping with the load and it may make the condition worse over time. If pain is kept below a 4/10 during and after exercises and the pain is allowed to settle between bouts of exercise, the tendon will likely adapt, get stronger and tolerate more activity with less pain in the future.
5. Stretch your tendon
Stretching your tendon places it under high compressive load. We now know that compressive load can be harmful to a painful tendon and may slow down its recovery. There is also no published evidence to support stretching as a useful intervention in tendon pain.
6. Massage your tendon
An overloaded and irritated tendon is often further aggravated by the compressive load of massage. Massage, like other passive therapies is not usually helpful in the long term, though may provide short term pain relief.
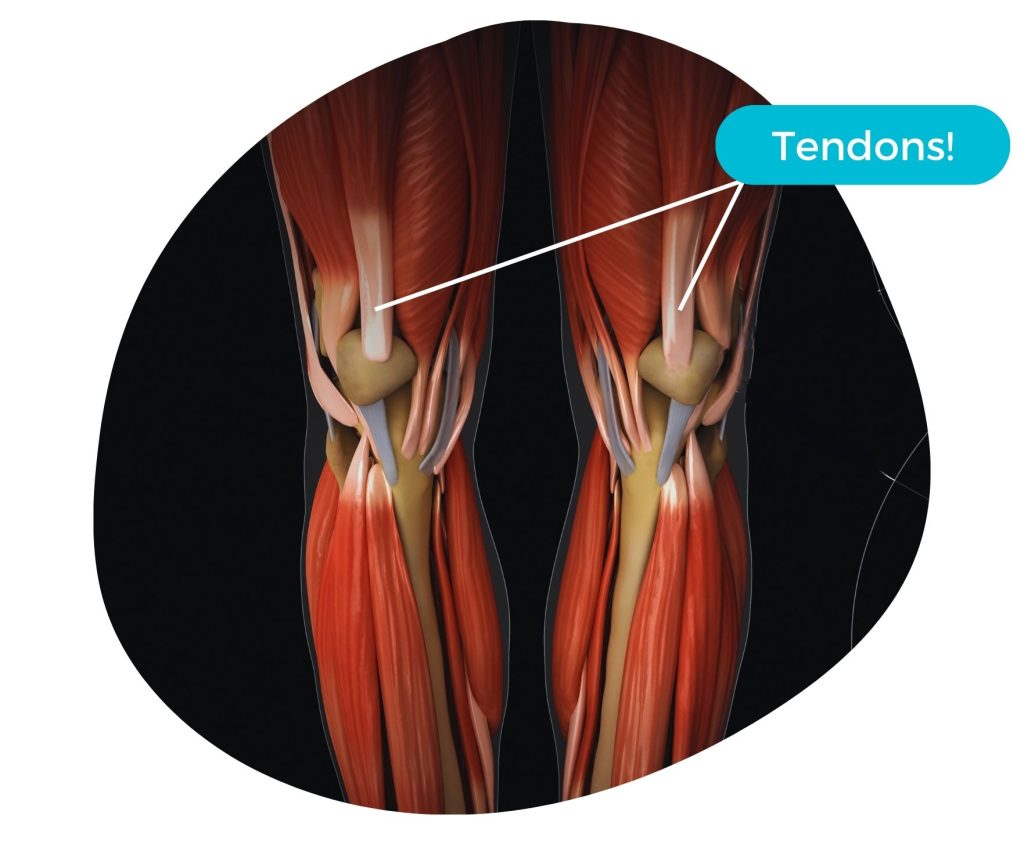
7. Be worried about the images of your tendon
Tendon imaging (ultrasound or MRI) and medical terms such as ‘degeneration’ and ‘tear’ can create some fear around loading a tendon. The concern is that loading may make the tear worse and cause further degeneration. There is actually evidence demonstrating that problematic tendons can eventually tolerate quite significant load without pain, especially when load is incrementally increased. Interestingly, the amount of changes identified on imaging is actually poorly associated with the load capacity in a tendon.
8. Be worried about rupture
Pain is a protective mechanism that makes you unload a tendon – therefore you are actually less likely to rupture a tendon which is painful. Most tendons that rupture are pain-free, despite having substantial pathology when subjected to medical imaging (see point 7 – imaging is not a reliable indicator of a tendons capacity!)
9. Take short cuts with rehabilitation
Time is required to develop strength and increase a tendon’s capacity. Although this time can seem long (sometimes 3-6 months or longer), the long-term outcomes are good if rehabilitation is completed. Things that are often promised as immediate fixes (see points 2 and 3) may provide short term pain improvements with no positive effect on long term tendon loading capacity and function.


10. Not understand tasks requiring high tendon loads
As a general rule, painful tendons hate being compressed and contracted forcefully from a stretched position. For the achilles and patella tendon, this involves spring like tasks, such as jumping, sprinting and changing direction. Early tendon rehab involves slow resistance exercises with gradual increases in load. As your tendon adapts to rehab, you should progress towards faster, spring like actions to prepare you for the functional demands of the muscle-tendon unit.
—-
So what does this mean for you?
The current best evidence for rehabilitating painful tendons is an exercise-based program which is progressive and guided by a physiotherapist with an understanding of these tendon loading principles. An individual’s pain and function need to be considered, and loads adjusted accordingly to ensure that tendons are being appropriately challenged.
—-
This blog is an adaptation of the work of Professor Jill Cook – a world leader in tendon pain management – and you can find her original article, along with an accompanying video at http://semrc.blogs.latrobe.edu.au/10-things-not-to-do-if-you-have-lower-limb-tendon-pain/.
—-
Stay tuned for more information about tendinopathy in our upcoming tendon series.
If you or someone you know is suffering from tendon pain, contact us:
Ph: (02) 49216879
E: admin@numovesphysiotherapy.com.au


 ????
????  Injury Prevention: Ignoring holiday niggles could lead to serious problems throughout your sporting season. Get any discomfort assessed, diagnosed and rectified early to avoid complications throughout the year.
Injury Prevention: Ignoring holiday niggles could lead to serious problems throughout your sporting season. Get any discomfort assessed, diagnosed and rectified early to avoid complications throughout the year.  Precision Preseason Training: Ensure your pre-season training is relevant, safe and optimal for you. We can work with you to tailor your training plan to your specific needs!
Precision Preseason Training: Ensure your pre-season training is relevant, safe and optimal for you. We can work with you to tailor your training plan to your specific needs! Faster Recovery: If you saw a lot of the sideline in 2023, ensure you get on top of your injuries early. Old injuries have a funny way of coming back if they are not looked after properly!
Faster Recovery: If you saw a lot of the sideline in 2023, ensure you get on top of your injuries early. Old injuries have a funny way of coming back if they are not looked after properly! Consistent Support: From preseason to game day, continuity of care can elevate your performance. Ongoing care ensures you’re on track, and any hurdles are addressed promptly, so you can focus on giving your best on the field.
Consistent Support: From preseason to game day, continuity of care can elevate your performance. Ongoing care ensures you’re on track, and any hurdles are addressed promptly, so you can focus on giving your best on the field. Maximise Your Potential: Physiotherapy isn’t just for recovery; it’s for optimisation! Ensure you’re getting the best out of your body with the best in physiotherapy care!
Maximise Your Potential: Physiotherapy isn’t just for recovery; it’s for optimisation! Ensure you’re getting the best out of your body with the best in physiotherapy care!

 Do seek professional guidence from your physio if you suspect you are dealing with tendinopathy. We can provide personalised advice and treatment options tailored to your specific needs.
Do seek professional guidence from your physio if you suspect you are dealing with tendinopathy. We can provide personalised advice and treatment options tailored to your specific needs. Don’t Stretch a Painful Tendon: Stretching can aggravate the condition and potentially worsen the pain. Instead, focus on gentle movements that promote mobility in the surrounding muscles and joints.
Don’t Stretch a Painful Tendon: Stretching can aggravate the condition and potentially worsen the pain. Instead, focus on gentle movements that promote mobility in the surrounding muscles and joints.






