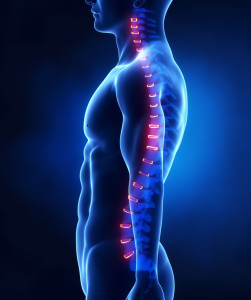
When it comes to sports injury management, most people are familiar with the old acronym RICE (rest, ice, compression, elevation) for soft tissue injury management, but what is the evidence for it, and can we do better?
Complete rest is rarely necessary following simple soft tissue injuries. For example, following a simple ankle sprain, a person who continues to move the ankle and weight bear as tolerated will have accelerated recovery compared to someone who avoids weight bearing and keeps the ankle still.
Ice is often used immediately following a soft tissue injury. Ice does not reduce swelling. If applied correctly, ice can reduce the temperature of surrounding tissues enough to reduce the nerve’s ability to carry information back to the brain, thereby reducing pain. Unfortunately, ice can interrupt the natural inflammatory response following an injury and possibly delay the healing response. The consensus is: only ice following an injury if the pain is intolerable – then ice it properly by making a bag of crushed ice and water.
The new recommended acronym for soft tissue injury management. PEACE (Protect, Elevate, Avoid anti-inflammatories, Compress and Educate) refers to the steps immediately following injury. In the next few days, the injury needs a bit of LOVE (Load, Optimism, Vascularisation and Exercise). For more information on how to best manage your injury, contact us on 49216879 or admin@numoves.com.au
For the full article visit the BJSM editorial: https://bjsm.bmj.com/content/54/2/72