How do you know if your bed mattress is contributing to your back pain?
How do you know if your bed mattress is contributing to your back pain?
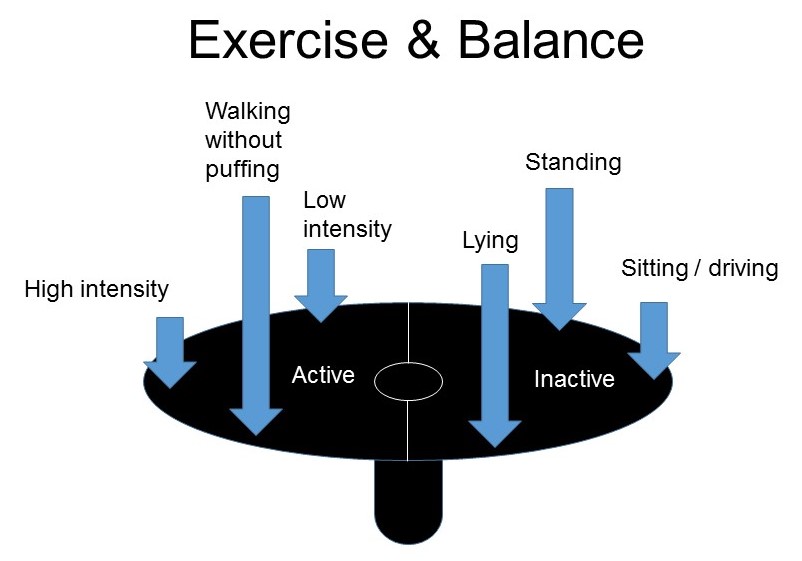
If you are like most people, you will spend 6-8 hours in bed each day. If your mattress is providing insufficient support for your back, it can aggravate or cause you back pain.
 A mattress with poor support allows your spine to rest in an abnormal position and alters stress on the discs, joints and soft tissue in and around the spine. This can cause pain and stiffness. Identifying if the mattress is a contributing factor for a back problem is an important step in overcoming the problem.
A mattress with poor support allows your spine to rest in an abnormal position and alters stress on the discs, joints and soft tissue in and around the spine. This can cause pain and stiffness. Identifying if the mattress is a contributing factor for a back problem is an important step in overcoming the problem.
So how do you know if your mattress is causing or aggravating you back problem? Here are some simple points to consider:
- If you wake up feeling stiff and sore most mornings this can point toward the mattress as a contributor
- Sleep in a different bed as a trial, preferably one with more support, and see if you feel less pain and stiffness
A mattress doesn’t last forever. Flipping your mattress regularly can help maintain your mattress but care is required in doing this. Having said this, sooner or later you may need to purchase a new one. If your mattress is contributing to your back pain you should look for a high quality orthopaedic mattress. Most bedding stores or bedding departments can advise you about mattress quality.
If its not the mattress then you need to see your physio and be assessed.