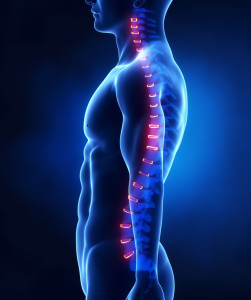
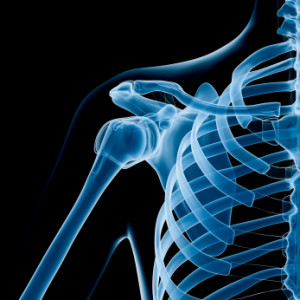
As physiotherapists and exercise physiologists, we help people address the neuro-musculoskeletal system (nerves, muscles, bones and joints) of the body with physical exercise strategies. This is reliant on a person getting involved with our recommended strategies and advice. The biggest barrier to not getting involved is time available and prioritising. Even when it actually makes us feel better to go for a walk or do a stretch, the time available often gets in the road.
As physiotherapists and exercise physiologists, we help people address the neuro-musculoskeletal system (nerves, muscles, bones and joints) of the body with physical exercise strategies. This is reliant on a person getting involved with our recommended strategies and advice. The biggest barrier to not getting involved is time available and prioritising. Even when it actually makes us feel better to go for a walk or do a stretch, the time available often gets in the road.
Physical balance is similar to nutrition advice. We know a balanced diet will make you feel better – so will finding a balance in exercise and movement. This balance changes throughout each week, month and year of our life but keeping a routine amount of the right type of activity for you will increase your feeling of well-being and reduce the risk of many health conditions such as diabetes and heart disease.
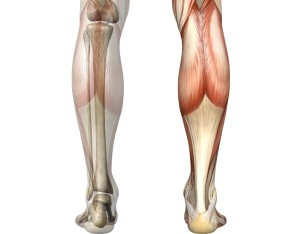
Most commonly it is too much sitting and not enough out of the chair activity that creates problems. Other times it is too much running and not enough recovery.
The message we commonly convey to our clients is:
Why do you exercise, why don’t you exercise, how much activity do you do, how does the activity levels weigh up against the amount you sit? The body will respond to the loads you put on it; similarly it will respond to what you eat and how much stress you are under.
Find the balance:
Consider what activity makes you feel good and write down a plan to achieve it. There is no better time to do it than today! Remember, it’s not always about doing more – some of you will be overdoing exercise for your own reasons – in this case finding the balance might be going for a swim or a walk instead of a run.